Eating Disorder Therapy
My approach to treating eating disorders is individualized, patient, collaborative, and humor-infused when appropriate. I work with individuals with eating disorders ages 17+. I utilize U.S. evidence-based modalities of CBT, ACT, DBT, ERP, and Motivational Interviewing, paired with internationally approved evidence-based interventions of psychodynamic and attachment approaches. I do not provide outpatient FBT treatment support, and can provide referrals for excellent FBT providers, if that is what you’re seeking for your child at this time.
I treat most types of eating disorders including Anorexia Nervosa, Bulimia, Binge-eating Disorder, and Orthorexia, as well as atypical presentations (Otherwise Specified Feeding and Eating Disorders) which are eating disorders that do not fit perfectly into one of the previous categories. These include Purging Disorder, Atypical Anorexia, and Night Eating Syndrome.
Diagnostic Eating Disorder Evaluations
If you are interested in participating in a comprehensive diagnostic eating disorder evaluation, please reach out to me. This is a stand-alone service I provide with no continuing therapeutic commitment expected or required. Continuing care and level of care treatment recommendations are provided upon completion of this evaluation.
What is an Eating Disorder?
An Eating Disorder (ED) is a persistent, intrusive, and distressing mental health condition centered around a person’s relationship with food and body. An eating disorder is both a mental and a physical illness. Eating disorders are accompanied by psychological disturbance and impairment of adaptive functioning. Mental fixations around weight, health, food, and body shape drive eating disordered behaviors, which can greatly compromise a person’s organ functioning, digestive tract, vitals, dental and esophageal health, and bone strength.
Eating disorders have been found to be derived from factors related to environment, social and cultural profile, genetics, and psychological vulnerabilities related to personality and temperament.
Eating disorders often co-occur with mood and anxiety disorders, perfectionism, devaluation of self, obsessive-compulsive disorder, substance use disorders, ADHD, or trauma. Eating disorders are often driven by obsessional and distorted thinking, as well as ritualistic or compulsive behavioral responses. This is notedly similar to OCD, and sometimes the eating disorder is largely derived from a preceding and primary OCD diagnosis.
Eating disorders are diagnosed in individuals of all body shapes and sizes, and from diverse ethnic, cultural, age, religious, and socioeconomic backgrounds. Eating disorders can be fatal with research finding one death per hour attributable to complications related to disordered eating.

The Thinking Behind Eating Disorders
Disordered eating thinking is embodied by a mental preoccupation with food, weight, calories, exercise, and/or dieting. ED thoughts sound judgmental, self-critical, and obsessive. Distorted thinking stemming from an eating disorder suggests that once a person achieves or maintains a certain body size, they will feel happy, desired, accomplished, worthy, or be at peace with themselves.
An eating disorder might sound like:
“I can’t eat unless…all the foods are “safe”; unless… I work out; unless… I stay under a certain calorie intake; unless...I maintain a certain weight, etc.”
“Other people skip meals, eat less than me, or are smaller than me, so I can’t be disordered.”
“I’m not sick enough, thin enough, or severe enough to have an eating disorder.”
“I don’t deserve to eat.”
“If I lose weight, I will be confident enough to date.”
“I live in a larger body with which I want to find peace, but I still feel fat phobic.”
“When I achieve my goal weight, then I will be happy.”
“I’m fat…I’m ugly… I’m lazy.”
“If I can change my body, I will be good enough, thin enough, right enough.”
“I ate too much / imperfectly yesterday, so now I can’t eat today or need to eat perfectly.”
“I didn’t eat perfectly at that meal, so the rest of the day’s eating is ruined.”
“My worth revolves around my weight (and the world tells me so).”
What Do Eating Disorder Behaviors Look Like?
Food/Drink Rules: rules that oversee safe and unsafe foods/drinks; safe and unsafe times to eat/drink; safe and unsafe settings in which to eat/drink; safe and unsafe circumstances in which to eat/drink
Food/Drink Rituals: rituals that oversee the why, when, and how the food/drink rules are applied
Exercise Rules
Exercise Rituals
Loss of control eating or emotional eating
Ongoing or failed attempts to reduce or control body size solely through food intake or exercise regimen
Increased avoidance or difficulty with communal, public, or celebratory eating
Body checking or body avoidance
Purging
Misuse of diuretics, laxatives, or weight-focused drugs
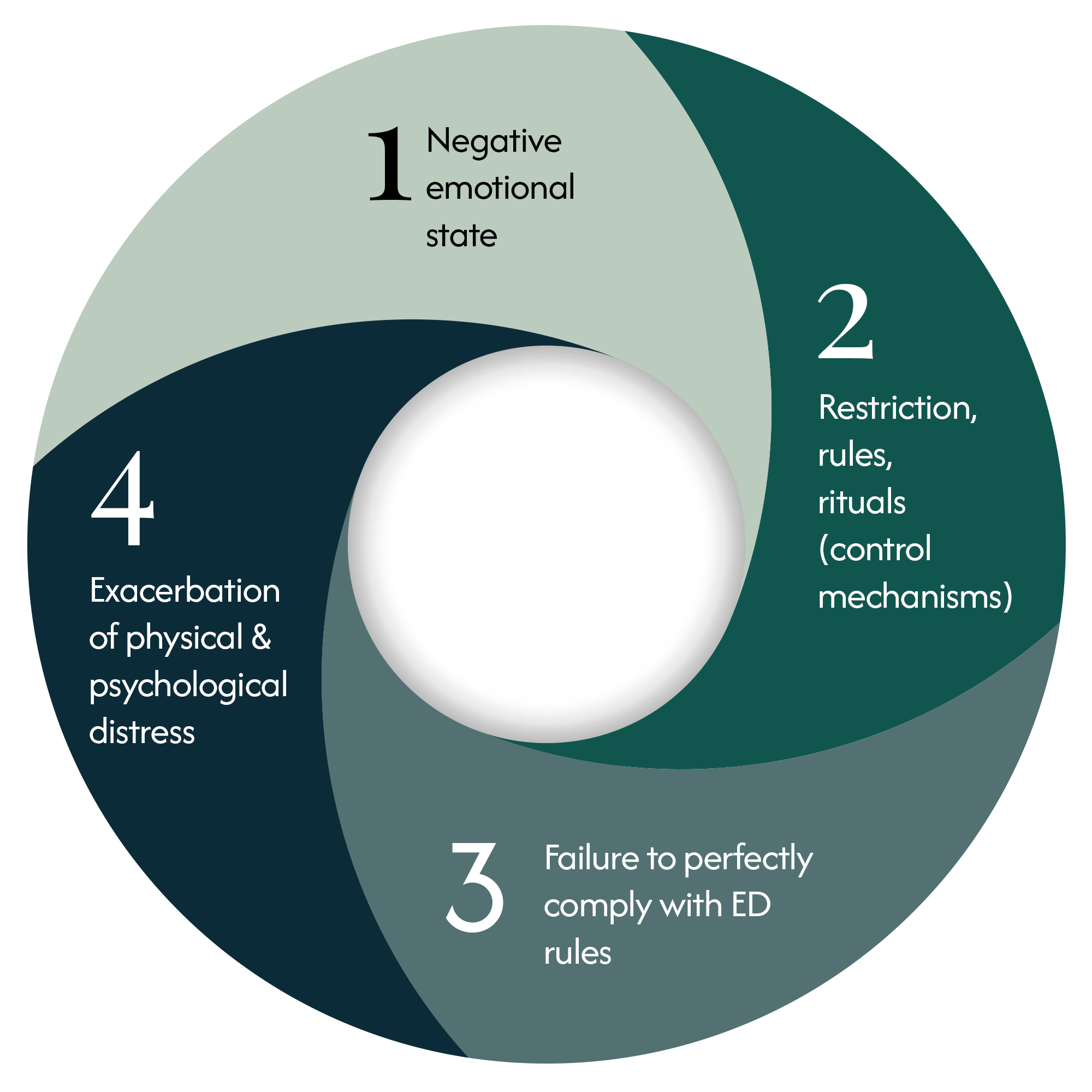
The Eating Disorder Cycle
When a person afflicted with an eating disorder experiences self-devaluation or negative emotional states (sadness, frustration, disgust, weakness, guilt, remorse, shame), they are prompted to respond using disordered behaviors intended to regulate or alter their unwanted feelings.
The eating disordered sufferer responds using control mechanisms rooted in various food or exercise-related rules, restriction, and rituals.
These behaviors may “work” at times, but cumulatively exacerbate and perpetuate psychological distress and emotion dysregulation, leading the person back to self-devaluation and negative emotional states.
Negative emotional state / self-devaluation / lack of control
Restriction, rules, rituals (control mechanisms)
Failure to perfectly comply with ED rules (eat imperfectly / binge / miss a workout)
Exacerbation of physical and psychological distress
And the cycle continues.
Eating Disorders by the Numbers
Approximately 10% of the general population (across gender) and 20% of women under age 50 will struggle with a clinically diagnosable eating disorder in their lifetime.
Only 15% - 20% of these individuals will receive treatment for their eating disorder.
Eating disorders are associated with the second highest mortality rate of any mental health condition, close behind the highest mortality rate that is represented by individuals with opioid use disorder.
Deaths are caused by a variety of medical (organ) failures associated with malnutrition; electrolyte imbalances causing sudden death for individuals engaging in regular purging behavior; and suicide.
More than 10,000 U.S. deaths per year are directly assigned to the presence of an eating disorder.
Anorexic individuals are 521% more likely to experience premature death than the general population.
For females aged 15-24, the mortality rate is 12x higher than all other causes combined.

Myths & Misconceptions About Eating Disorders
Eating disorders only occur in persons of white, thin, or socioeconomic privilege
Eating disorders only occur in cis-women
Eating disorders are not serious illnesses
Eating disorders only develop in individuals at or older than adolescence
Binge eating disorders only present in higher weighted individuals
Eating disorders require a weight criteria
Eating disorders are only about food/eating/weight
Eating disorders are only the result of learned behavior (the parent is at fault)
Eating disorders can be visually “seen”
Eating disorders cause weight change
Eating disorders are a choice
Any dieting individual
Military & Veterans (1 out of 3 women and 1 out of 5 men)
Individuals living with food insecurity
BIPOC population (drastically under-identified/diagnosed)
Vegan and vegetarian-adherent individuals
LGBTQIA+ population, especially transgender and non-binary individuals
Competitive athletes
Individuals engaging in excessive social media use
Women-identified individuals
Rural Americans
Trauma survivors
Living in an environment with high pressure placed upon performance, grades, success, or appearance
Eating Disorders: Vulnerable Populations
To learn more about the truths of Eating Disorders and to take the first step toward freedom from this disorder, please reach out to begin your recovery journey with me.
What Can I Expect from Eating Disorder Treatment with Sara Watts?
My approach to treating eating disorders is collaborative and adaptable.
Eating disorder recovery achieves its best outcomes when treated using a multidisciplinary approach, including psychotherapy, nutritional counseling, medical monitoring, and medication. Research varies regarding the direct impact of the therapeutic relationship on eating disorder recovery, but no research disputes that therapeutic intervention increases the probability of an improved or full recovery from eating disorders. When left untreated, eating disorders like most mental health disorders, progress and become more chronic and pervasive.
Ambivalence is natural and expected. If you need a slower approach, I can accommodate that, and if you need a more direct and challenging approach, I can accommodate that as well. We will apply cognitive, behavioral, and mindfulness-based interventions incorporating thought awareness and deconstruction, skills-based tools, and exposure exercises (to challenge rules, rituals, and rigidity). We will also take into consideration the origins, developmental contributors, and perpetuating factors of your unique eating disorder journey and narrative.
No step is too small to make when approaching working on an eating disorder. Starting anywhere at all is progress as compared to passively or intentionally surrendering to the eating disorder condition.

HAES Approach to Eating Disorders
I am a Health At Every Size (HAES) practitioner. This means I work from a therapeutic foundation that is anti-diet, weight inclusive, and supportive of the biological (and positive!) reality of body diversity.
I work to therapeutically support holistic health enhancement. This means we will examine and attend to ALL of your needs (physical, social, spiritual, economic, and emotional). I promote life-enhancing movement, which means engagement in physical activity that is enjoyable, not dreaded or compulsory.
I am fully aware of my own weight biases, and choose to live and work from a place advocating for the end of weight stigma and discrimination.
As a HAES provider, I work with eating disordered individuals using an approach of eating for well-being. This means we approach food work with an initiative of balancing not just nutritional needs, but also food accessibility, hunger, satiety, and pleasure.
Learn more about my approach to HAES →
Learn More About Eating Disorder Therapy with Sara Watts
If it would help, I would be pleased to offer a 15 minute complimentary call to introduce myself and my approach to eating disorder therapy.
Please feel free to contact me today.

Eating Disorder Resources
Recommended Reading
The Anti-Diet, Christy Harrison
Life Without Ed, Jennie Schaefer
Fearing The Black Body, Sabrina Strings
The F*ck It Diet, Caroline Dooner
Body Kindness, Rebecca Scritchfield
Midlife Eating Disorders, Cynthia Bulik
The Wellness Trap, Christy Harrison
Sick Enough: A Guide to the Medical Complications of Eating Disorders by Jennifer Gaudiani, MD, CEDS
The Body Is Not An Apology, Sonya Renee Taylor
Broken Mirror, Katharine A. Phillips (Body Dysmorphic Disorder)
Health At Every Size, Linda Bacon
Intuitive Eating, Evelyn Tribole & Elyse Resch
The Parent’s Guide to Eating Disorders, Marcia Herrin & Nancy Matsumoto
Fat Talk: Parenting in the Age of Diet Culture, Virginia Sole-Smith
Helplines
ANAD Helpline:
(888)-375-7767
(M-Fri, 9am-9pm CT)
Crisis Text Line: Text “Talk” to 741-741
National Alliance for Eating Disorders:
(866)-662-1235
(M-Fri, 9am-7pm ET)
Diabulima Helpline: (425) 985-3635
https://www.diabulimiahelpline.org/
Podcasts
Food Psych - Christy Harrison, RD, CEDS
Real Health Radio - Seven Health
Maintenance Phase - Aubrey Gordon & Michael Hobbes
*Some triggering content due to weight numbers, so please listen only when it is appropriate in your recovery
Resources
National Eating Disorders Resource Center:
https://www.nationaleatingdisorders.org/resource-center/
Eating Disorders in LGBTQIA Populations (National Center):
https://www.nationaleatingdisorders.org/eating-disorders-in-lgbtqia-populations/
Association for Size Diversity and Health:
https://asdah.org/events
Resources for Loved Ones
NEDA Parent Toolkit:
https://www.nationaleatingdisorders.org/toolkits/
Families Empowered and Supporting Treatment of Eating Disorders:
https://feast-ed.org