OCD & Anxiety Disorder Therapy
My approach to treating Obsessive-compulsive disorder (OCD) and Anxiety disorders is collaborative, insight-focused, and patient. Changing ways of thinking and doing that are often times well-practiced for years and even decades is hard work. Any change or willingness to look at or do something in a different way than you have before should be recognized as a great success.
OCD, like many mental health disorders, originates within both genetic and environmental constructs. Why and how you developed your way of thinking is not irrelevant. Evidence-based approaches, often championed and required by insurance companies, deter us from spending too much time on predispositional factors and formational experiences. However, these factors and experiences represent you as a whole, and not just a sum of your “OCD parts”.
In my therapeutic practice, I offer an opportunity for you to be seen both effectively and holistically.
I will typically begin our work by providing a heavy dose of psychoeducation. I then apply evidence-based therapies primarily utilizing ERP, ACT, and CBT interventions, at times supplementing with psychodynamic and attachment-based approaches for clients who feel stuck on or curious about the development of their disorder.

What are the Differences Between OCD and Anxiety?
OCD
OCD is a mental health condition characterized by unwanted, persistent, distressing, and intrusive thoughts, images, or urges (obsessions).
These thoughts elicit responses (rituals) composed of repetitive behaviors or mental acts (compulsions). The OCD cycle causes significant distress, anxiety, and discomfort. OCD at its core is a “doubting disorder”.
Anxiety Disorders
Anxiety Disorders are characterized by symptoms of persistent worry, restlessness, feeling on edge, sleep and/or appetite disturbances, and difficulty concentrating or being present.
Anxiety Disorders can manifest in variant diagnostic presentations including phobias, generalized anxiety, social anxiety, panic, separation anxiety, agoraphobia, and selective mutism.
Diagnostic OCD Evaluation
If you are interested in participating in a comprehensive diagnostic OCD evaluation, please reach out to me. This is a stand-alone service I provide with no continuing therapeutic commitment expected or required. Continuing care and level of care treatment recommendations are provided upon completion of this evaluation.
The OCD Cycle:
Arrival of an obsessional thought, related to a core fear, a feeling of “not just right”, or a feeling of disgust
Responsive compulsion to fix, alleviate, or remove the discomfort of that thought or feeling
Achievement of a temporal feeling of relief, peace, or accomplishment
Belief is reinforced that an obsessional thought must be answered with a responsive compulsion
And the cycle continues.
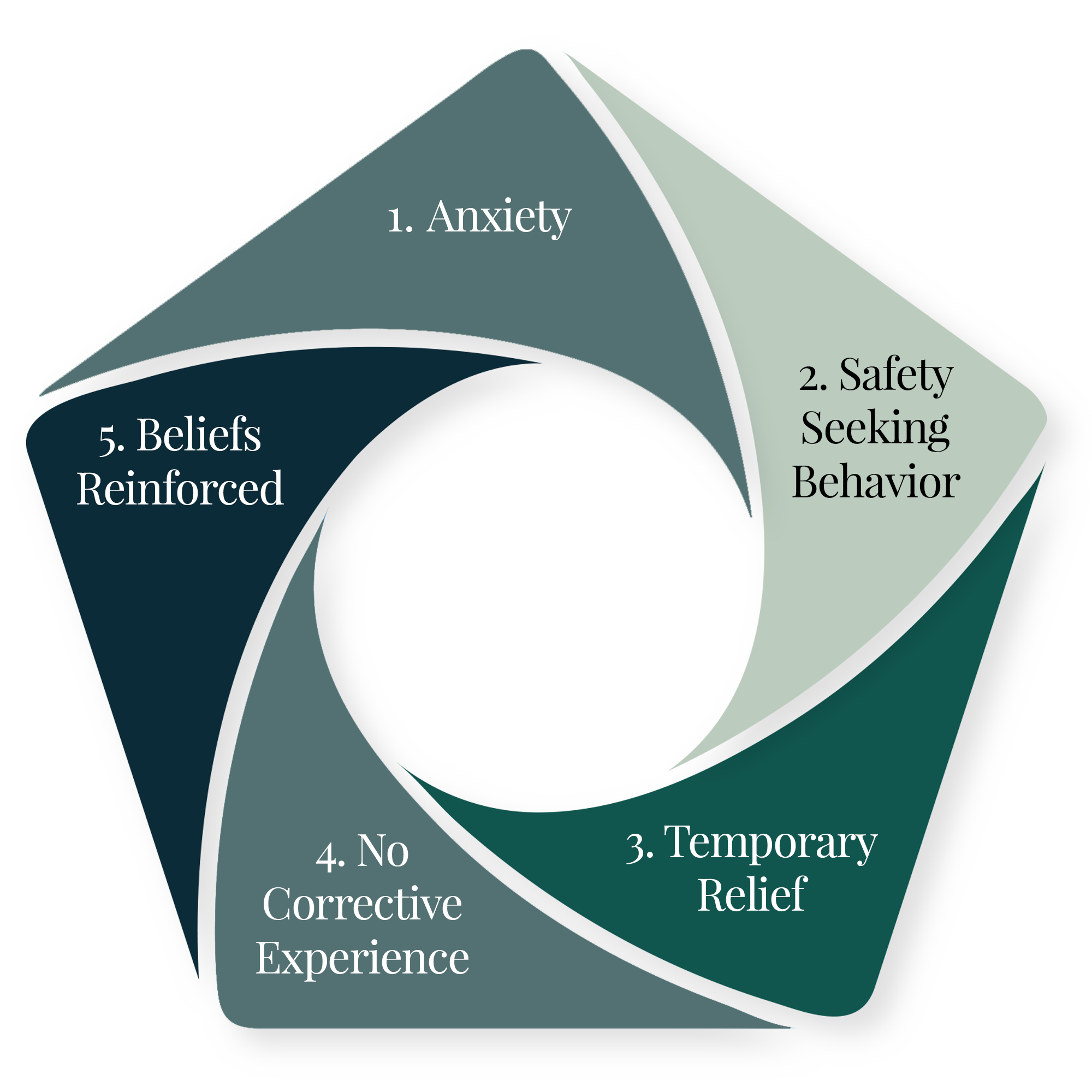
The Anxiety Cycle:
Anxiety (notable physiological sensations + thought: “something is wrong”)
Safety-seeking behavior to reduce feeling of anxiety (avoidance, reassurance-seeking, rumination, review, problem-solving)
Temporary relief from feeling of anxiety
No corrective experience (absence of learning that anxiety is not in fact dangerous and that safety-seeking behaviors are unnecessary and unproductive)
Belief is reinforced that safety seeking behaviors are necessary and productive in order to “be ok”
And the cycle continues.
Together, we will begin to disrupt these cycles. We will collaboratively determine what is most effective for you and your individual OCD or anxiety presentation.
Understanding OCD
A person afflicted with OCD feels driven to respond to the obsession using a compulsion in order to neutralize or mitigate the anxiety associated with the obsession. Compulsions can feel as though you are not free to act as you might otherwise choose. However, compulsions only provide temporary relief, and perpetuate the OCD cycle. If left untreated, OCD can significantly compromise and deteriorate daily life, functioning, and relationships.
OCD is often greatly misunderstood, its name misused, and its impact on sufferers devalued by non-clinical stereotypes referring to people simply being overly attentive to organization or cleanliness. “Type A” people are not the same population as those living with OCD, though there may be overlap between the two populations and in some instances, shared traits.
OCD’s “stickiness” is not coincidental. OCD often targets what you most value such as health, relationships, morality, faith, self-image, or your relationship with food/body. Remember: the key components qualifying a thought as obsessional are that it is distressing, intrusive, and negatively impacting (or compromising) day to day functioning.
Because OCD is very smart, it vigilantly competes for prime cognitive real estate within the minds of often very smart inhabitants. Both OCD and folks who have OCD are uniquely qualified in rationalizing irrational beliefs, behaviors, and rituals.

OCD obsessions might sound like:
“I need to ensure they know that I love them or that they love me.”
“I need to be perfect.”
“I am a bad/terrible/evil person for having that thought.”
“I need to do things this way, or something bad will happen.”
“I need to ensure that I am or others are ok / are unharmed / are safe.”
“I need to protect myself and/or my loved ones from getting sick.”
“What if I’m not who I think I am?” (can relate to morality, religion, violence, sexuality, relationships)
“I need to ensure that things look, sound, feel “‘just right’”.
“I need to ensure I don’t forget anything.”
Just about anything! Remember, OCD is super smart and creative and will shape-shift in a myriad of ways to attract your attention.
OCD compulsions might look like:
Checking behaviors
Rumination (the most common mental compulsion)
Rearranging, cleaning, or ordering to achieve a “just right” feeling (applies to objects or your physical body, senses, position)
Reassurance Seeking
Repetitive behavior, i.e. tapping, counting, repeating, praying
Ritualistic behaviors (differentiate from routines due to being accompanied by obsessional thought)
Avoidance (a passive and yet active compulsion to eliminate or reduce the distress of the obsessional thought)
OCD by the Numbers
1 in 40 adults and 1 in 100 children meet criteria for clinical diagnosis
80% of OCD cases onset either between ages 7-12yo and by age 14 (early onset), or between 18-24yo (early adult onset)
China has the highest OCD prevalence
OCD affects 1-3% of the global population
Cis-males are more likely to experience OCD onset in childhood (9-11yo) vs. cis-females being more likely to experience OCD onset in early adulthood (21-24yo) **these statistics are likely influenced by both gender-norming and gender-conforming behaviors, i.e. identifying young boys presenting with OCD presentations as “atypical” vs. young girls with the same symptomatology; or, symptom suppression resulting in delayed diagnosis for young girls due to their higher predisposition to successfully mask or “manage” their OCD symptoms
The average number of years between OCD onset and receiving proper OCD diagnosis is 9-17 years. This is in part due to patient disclosure fear and shame, provider misdiagnosis, and an overall lack of OCD-specialized healthcare providers

Myths & Misconceptions About OCD
OCD is just an issue with cleanliness, germs, or organization
OCD is a lifestyle choice or personality trait
OCD is specific to certain ages, gender, ethnicity, or socioeconomic status
OCD affects “everyone” at least a little or at some point (i.e. “I’m so OCD about…”)
OCD is just over-active anxiety, neuroticism, or being dramatic
OCD is untreatable
OCD: Vulnerable Populations
Family history of OCD
Pre-pubescent boys
Women in their 20’s
Post-partum women
Childhood trauma survivors
Individuals living with chronic stress
Perfectionistic individuals
Substance users
How is OCD Different from OCPD?
Most often what people think of when they think of OCD, is actually more accurately related to the diagnosis of Obsessive-Compulsive Personality Disorder (OCPD).
OCPD is characterized by a pervasive preoccupation with order, control, hyper-attunement to detail, and perfectionism. OCPD is not associated with compulsions, despite its name insinuating this. Approximately 20% of people can have both disorders.
People with OCPD may be experienced as rigid and inflexible. They typically hold others to their same specific standards of thinking and behaving, which can often cause relational strain or loss.
Treatment areas of focus for those with OCPD will focus on increasing openness and flexibility, as well as the capacity to delegate. Additional areas of treatment focus may be reducing an excessive over-valuation on the importance of work and work performance, as well as the conviction that there is only a right or a wrong way to think, feel or act.

OCD vs. Generalized Anxiety Disorder
Although a person can have both Generalized Anxiety Disorder (GAD) and OCD, these diagnoses have distinctive differences. Reductively, we consider GAD as being a “worrying” disorder and OCD as being the “doubting” disorder.
GAD is best characterized by persistent and pervasive worry, contained most often to reality-based and everyday life experiences. Although GAD creates a distressing thinking cycle, GAD does not commonly elicit a compulsive or ritualistic response in order to mitigate the distress. Additionally, GAD does not necessarily produce unwanted thoughts. GAD thoughts might feel more realistic, practical, productive, or rationalized as compared to OCD thoughts.
Sometimes, GAD and OCD can elicit similar responses such as reassurance-seeking, rumination, and avoidance, but GAD is less selective and less consistent regarding how it responds to anxious thoughts. It is a predictable but not a ritualistic cycle.
Another distinctive difference is that GAD is ego-syntonic while OCD is ego-dystonic. When a condition is ego-syntonic it means it is experienced as being aligned with the self. When a condition is ego-dystonic, it is experienced as a conflict between the self and the disorder. A person with GAD is not internally conflicted by the content of their anxious thoughts. They are struggling with the feeling of anxiety, but they also accept and often even value what they are having anxiety about. In contrast, a person with OCD feels their disorder compromises and even contradicts their sense of self and values.
Learn More About OCD & Anxiety Disorder Therapy with Sara Watts
If it would help, I would be pleased to offer a 15 minute complimentary call to introduce myself and my approach to OCD & Anxiety Disorder therapy.
Please feel free to contact me today.

OCD & Anxiety Resources
SUPPORT GROUPS, READING, & PODCASTS
Resources For Supporting a Loved One With OCD
Obsessive-Compulsive Disorder: A Guide for Family Friends and Pastors, Robert Collie, ThD
Obsessive-Compulsive Disorder: New Help for the Family, Herbert L. Gravitz, PhD
The Family Guide to Getting Over OCD: Reclaim Your Life and Help Your Loved One, Jon Abramowitz
https://beyondocd.org/information-for-friends-and-family/help-for-families-living-with-ocd